Appeals Management
URAC-Accredited Technology-Enhanced Processes Delivering Faster Resolutions
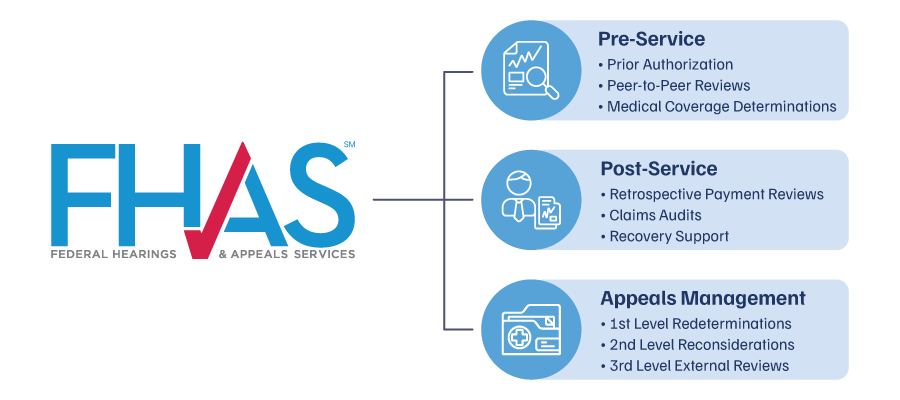
FHAS transforms complex healthcare appeals through automated, data-driven processes that accelerate resolution times and reduce administrative burden. Our tech-enabled platform and URAC accreditation ensure compliant, defensible decisions across commercial insurance, Medicare, Medicaid, and self-insured employer programs.
End-to-End Appeals Management
From initial intake to final determination, provide efficient 1st- and 2nd-level internal and 3rd-level external appeals for commercial insurance, Medicare, Medicaid, and self-insured plans with unprecedented efficiency.
FHAS revolutionizes appeals management by combining advanced automation with clinical expertise to eliminate backlogs and accelerate resolution outcomes across all health programs. As a URAC-accredited IRO, our automated workflows integrate regulatory compliance, clinical intelligence, and data-driven decision-support tools to deliver timely, defensible determinations that reduce administrative costs while improving accuracy across the entire appeals lifecycle.

Why Partner with FHAS?
URAC-Accredited Processes
As a URAC-accredited Independent Review Organization (IRO), our workflows ensure rigorous compliance standards and accelerated processing times.
Multidisciplinary Intelligence
Our physicians, nurses, and legal experts leverage advanced analytics and automated case routing for comprehensive clinical and regulatory reviews.
High-Volume Capability
Technology-enhanced processes manage thousands of appeals across all health programs, maintaining 100% compliance with measurable efficiency gains.
Comprehensive Appeals Management Services
Combined with our pre-service utilization and claims review, FHAS provides the full spectrum of review services from initial intake to 3rd-level external appeals. We offer appeals support for both 1st- and 2nd-level internal review as well as 3rd-level external appeals review. Our services integrate seamlessly into your workflows to manage grievances, medical necessity denials, and coverage disputes at any point in the appeal lifecycle.
Appeals Service Specialties
- Internal Appeals
Manage first- and second-level appeals with timely, well-documented case reviews that comply with regulatory and contractual requirements.
- External Review (IRO)
Deliver objective third-party reviews for coverage or medical necessity disputes, conducted by licensed, board-certified physicians.
- Grievance Processing
Intake, classify, and resolve member and provider grievances with clear documentation and adherence to CMS and ACA regulations.
- Timeliness Monitoring
Track appeal timeframes to ensure all reviews and notifications meet state and federal compliance standards.
- Clinical Review Support
Evaluate medical necessity, experimental/investigational services, and level-of-care decisions based on current evidence and guidelines.
- Peer-to-Peer Engagements
Coordinate physician-to-physician discussions to resolve complex denials and promote agreement on care appropriateness.
- Audit Preparation & Support
Prepare detailed appeal documentation to support external audits or oversight, reducing risk of sanctions or penalties.
- Custom Reporting
Deliver performance data and trend analysis to help clients monitor outcomes, identify denial patterns, and improve processes.
Improve Outcomes and Lower Administrative Burden
Operational
Efficiency
Automated workflows eliminate backlogs and free internal resources while accelerating resolution times through intelligent case management processes.
Regulatory Confidence
Automated compliance monitoring across commercial, Medicare, Medicaid, and self-insured programs eliminates audit exposure and regulatory penalties.
Resolution Improvement
Data-driven expert reviews deliver faster, defensible decisions that strengthen relationships with members, providers, and regulatory agencies.
Subscribe to the FHAS Insider
For the latest in medical review and IDR News