Medical Review
URAC-Accredited Technology-Enabled Services Delivering Measurable Results
FHAS eliminates healthcare inefficiencies through data-driven, tech-enabled medical review processes that have delivered proven results across millions of claims. Our automated workflows and dual URAC accreditation ensure cost reduction and regulatory compliance for commercial insurance, Medicare, Medicaid, and self-insured employers.
Intelligent Medical Review Operations
FHAS revolutionizes healthcare decision-making by combining advanced technology with clinical expertise to solve your most pressing operational challenges. Our automated, data-driven review platform ensures healthcare services meet the highest standards of appropriateness, accuracy, and compliance across diverse health programs including commercial insurance, Medicare, Medicaid, and self-insured employer plans.
With dual URAC accreditation in IRO and HUM and guidance from board-certified clinical professionals, FHAS provides the technological backbone and clinical authority healthcare organizations need to make confident, compliant, and cost-effective care decisions.

Why Partner with FHAS?
Dual URAC Accreditations
IRO and HUM accreditations combined with cutting-edge automation platforms ensure unmatched quality, compliance, and efficiency.
Clinical Intelligence
Board-certified physicians and clinical experts leverage advanced analytics for evidence-based reviews with unprecedented speed and accuracy.
Tech-Enabled Performance
Automated workflows processed millions of claims across all health programs, maintaining 100% timeliness while delivering measurable savings.
Comprehensive Review Specialties
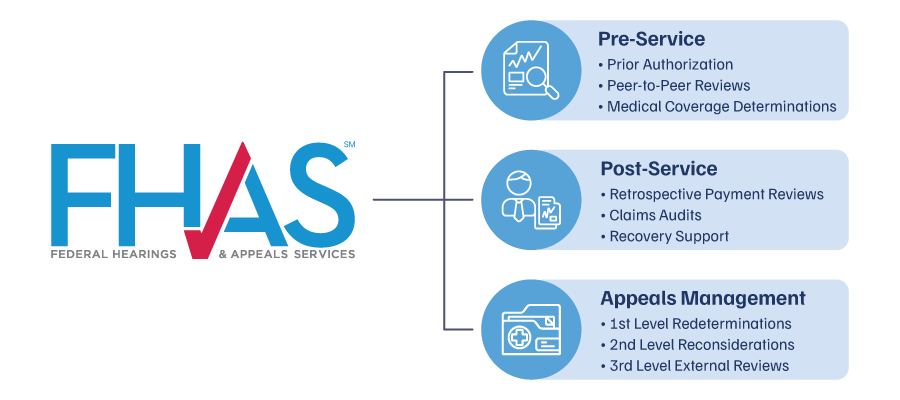
As a URAC-accredited IRO with Health Utilization Management (HUM) accreditation, FHAS provides tailored prospective, concurrent, and retrospective medical review services—seamlessly integrating into any stage of your internal or external claims process.
Review Specialty Services
- Medical Review
Validate coding, documentation, and medical necessity pre- and post-service to reduce errors and overpayments. - Pharmacy Review
Assess prescription claims for cost-effectiveness, step therapy alignment, and formulary adherence. - Behavioral Health
Review mental health and substance use claims against coverage policies and clinical guidelines.
- Outpatient Services
Evaluate outpatient physician claims for medical necessity, appropriateness, and policy adherence. - Inpatient Hospital
Analyze inpatient claims to confirm medical necessity, appropriate length of stay, and regulatory standards. - Hospice
Review end-of-life care claims to ensure appropriate services and accurate billing. - Malpractice
Provide objective clinical analysis to support fair resolution of liability disputes.
- Corporate Integrity Agreement Audits
Conduct independent oversight to meet regulatory and legal requirements. - Coding Audits
Audit medical coding for accuracy, adherence to standards, and error prevention. - Risk Management
Identify and address financial and regulatory risks through targeted reviews. - Provider Outreach and Education
Partner with providers to strengthen documentation and reduce denials.
Transform Your Operations with FHAS
Enhanced Efficiency
Tech-assisted prior authorizations, UM, and automated peer review routing accelerate decisions while eliminating workflow bottlenecks.
Quantifiable Cost Reduction
Data-driven analytics and automated fraud detection prevent inappropriate services, delivering millions in annual savings through prevention.
Risk Mitigation
Advanced compliance monitoring across all health programs eliminates audit exposure through proactive, automated quality assurance protocols.
Our Diverse Clients
FHAS supports a wide range of organizations with tailored medical review solutions
Subscribe to the FHAS Insider
For the latest in medical review and IDR News
