What goes into an arbitration decision? This question is routinely asked of parties, Congress, federal agencies, and consumer advocate groups. This very question has been the subject of multiple lawsuits as parties dispute the statutory text of the No Surprises Act and the U.S. Departments of Health and Human Services, Labor, and the Treasury (the Departments) promulgated rules.
Considerations by Arbitrators
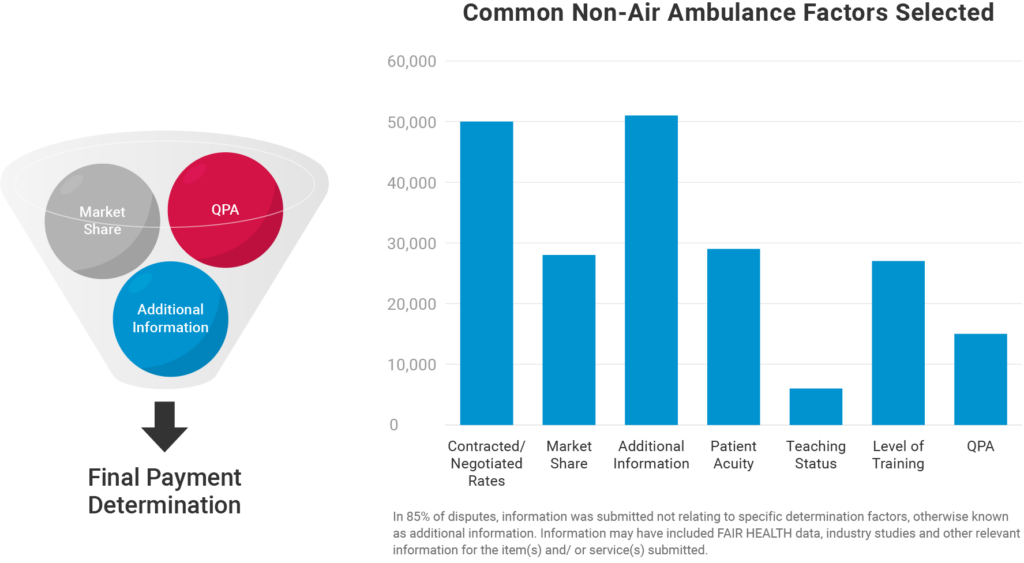
With the federal court rulings associated with TMA I, II, III, and IV, the methodology by which arbitrators make decisions shifts the focus of the arbitrator back to the original text of the No Surprises Act, in which arbitrators must “consider” multiple factors, including:
- QPA (qualifying payment amount)
- Additional information such as
- The level of training, experience, and quality and outcomes measurements of the provider or facility that furnished such item or service.
- The market share held by the nonparticipating provider or facility or that of the plan or issuer in the geographic region in which the item or service was provided.
- The acuity of the individual receiving such item or service or the complexity of furnishing such item or service to such individual.
- The teaching status, case mix, and scope of services of the nonparticipating facility that furnished such item or service.
- Demonstrations of good faith efforts (or lack of good faith efforts) made by the nonparticipating provider or non-participating facility or the plan or issuer to enter into network agreements and, if applicable, contracted rates between the provider or facility, as applicable, and the plan or issuer, as applicable, during the previous 4 plan years.
Important Points for Parties to Remember
- An arbitrator considers only the information provided in each dispute; an arbitrator cannot independently investigate a claim
- An arbitrator only selects either the IP or NIP offer – the arbitrator cannot replace its judgment in place of the parties and create a wholly unique payment amount
- FHAS arbitrators have decades of expertise in health claims review, analysis, and payment adjudication; they have completed arbitration courses sponsored by the American Health Law Association.
- Parties need to support their points with evidence and documentation that sufficiently demonstrates why an arbitrator should choose one offer over the other;
- An arbitrator cannot consider prohibited factors when making a payment determination including:
- Usual and customary charges
- Payments furnished under Medicare, Medicaid, CHIP, and Tricare
FHAS – Ready to Help
As parties navigate IDR, FHAS conducts regular status meetings with parties and provides an open line of communication with any party looking for more information on their pending disputes and determinations.
Throughout these meetings, common questions rise to the surface. Many providers and health plans alike are left with uncertainties and misunderstandings around the IDR process. As the most efficient IDRE among those certified to deliver dispute determinations under the No Surprises Act, FHAS aims to clear up these uncertainties to further improve the IDR process for parties..
Common questions we encounter include:
- “What are the main factors considered in an arbitration decision?”
- “Why are our objections being ignored?”
Leave a comment below with any additional questions you have that we can answer that would help you better understand the process and the factors that go into an arbitrator’s determination.
“What are the main factors considered in an arbitration decision?”
Different arbitrators may make a different determination. FHAS aims to be as consistent as possible in our determinations and is always open to providing the reason for the determination and evidence provided by the other party. This can be requested via email to idre@fhas.com or by submitting a message on our contact form.
Most importantly, the arbitrator considers only the information provided in each dispute.
“Why are our objections being ignored?”
When offers are requested — or even determinations reached — without a direct response to an objection, some parties have expressed frustration that their objections have gone unanswered and are not considered.
It’s important to know that objections from either party are never ignored. If the dispute proceeds through to the next phase of the process, typically the offer stage, the objection has been overruled. Parties are always permitted to request the reason for their objection being overruled, which FHAS facilitates quickly when requested via email to IDRE@fhas.com or our contact form.
Legal Disclaimer
The information contained in this content piece is for general informational purposes only. While we strive to ensure the accuracy and completeness of the information presented, we make no representations or warranties of any kind, express or implied, about the accuracy, reliability, suitability, or availability with respect to the content or the information, products, services, or related graphics contained in the content piece for any purpose. Any reliance you place on such information is therefore strictly at your own risk. The content of this page is subject to change without notice. The information provided in this document does not constitute legal or other professional advice, and is non-binding upon FHAS and any federal government agencies.
IDR Insider Newsletter
Subscribe to the FHAS IDR Insider newsletter to keep up will all IDR news.



Is Fair Health Data for Out of Network payments appropriate to provide for the arbitrator to reference?
Fair Health Data has not been explicitly stated as an impermissible or allowable determination factor for arbitration. However, CMS and Fair Health have announced plans to release an IDR-compliant Fair Health Database. In the absence of this, Fair Health data has been submitted by parties and is considered “additional information” by the arbitrator. In terms of the value applied by the arbitrator for Fair Health data of out-of-network payments, be sure to include what the Fair Health database being presented is based on (e.g. geographic region, timespan for services included etc.) to ensure the documentation best serves the item(s) and/ or service(s) being disputed.